Bladder cancer usually originates in the bladder lining, which consists of a mucous layer of surface cells called transitional epithelial cells, smooth muscle, and a fibrous layer. Tumors are categorized as low-stage (superficial) or high-stage (muscle invasive).
More than 90% of cases originate in the transitional epithelial cells (called transitional cell carcinoma; TCC). Then next most common type is squamous cell carcinoma caused by Schistosoma haematobium (parasitic organism) infection and is often times associated with a long standing urinary bladder stone. Rare types of bladder cancer include small cell carcinoma, carcinosarcoma, primary lymphoma, and sarcoma.
Bladder cancer is 2 to 3 times more common in men. Bladder cancer is the fourth most common type of cancer in men and the eighth most common type in women.

CAUSES AND RISK FACTORS
Cancer-causing agents (carcinogens) in the urine may lead to the development of bladder cancer. Cigarettte smoking contributes to more than 50% of cases, and smoking cigars or pipes also increases the risk.
Other risk factors include the following:
- Age
- Chronic bladder inflammation (recurrent urinary tract infection, urinary stones)
- Consumption of Aristolochia fangchi (herb used in some weight-loss formulas)
- Diet high in saturated fat
- Exposure to second-hand smoke
- External beam radiation
- Family history of bladder cancer (several genetic risk factors identified)
- Gender (male)
- Infection with Schistosoma haematobium (parasite found in many developing countries)
- Personal history of bladder cancer
- Treatment with certain drugs (e.g., cyclophosfamide—used to treat cancer)
Exposure to carcinogens in the workplace also increases the risk for bladder cancer. Medical workers exposed during the preparation, storage, administration, or disposal of antineoplastic drugs (used in chemotherapy) are at increased risk. Occupational risk factors include recurrent and early exposure to hair dye, and exposure to dye containing aniline, a chemical used in medical and industrial dyes.
Workers at increased risk include the following:
- Hairdressers
- Machinists
- Printers
- Painters
- Truck drivers
- Workers in rubber, chemical, textile, metal, and leather industries
SIGNS AND SYMPTOMS
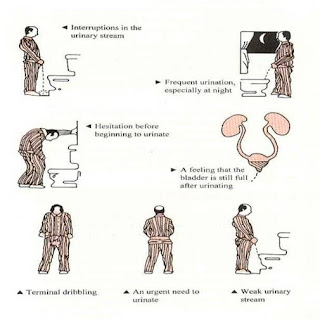
The primary symptom of bladder cancer is blood in the urine (hematuria). Hematuria may be visible to the naked eye (gross) or visible only under a microscope (microscopic) and is usually painless.Other symptoms include frequent urination and pain upon urination (dysuria).
DIAGNOSIS
Diagnosis of bladder cancer includes urological tests and imaging tests. A complete medical history is used to identify potential risk factors (e.g., smoking, exposure to dyes).
LABORATORY TESTS
- Urinalysis (to detect microscopic hematuria)
- Urine cytology (to detect cancer cells by examining cells flushed from the bladder during urination)
IMAGING TESTS
Ultrasound
This is the initial test performed and most patients come to the urologist with an ultrasound report.
More and more frequently computed tomography (CT) without and with intravenous contrast has replaced intravenous pyelography (IVP) the evaluation of hematuria. With computer-assisted reconstruction, longitudinal views of the urinary tract can now be made, although their sensitivity in detecting small or flat tumors of the urothelium is limited.
Intravenous Pyelography
If CT is not performed, IVP is indicated in all patients with signs and symptoms suggestive of bladder cancer. Urography is not a sensitive means of detecting bladder tumors, particularly small ones. However, it is useful in examining the upper urinary tracts for associated urothelial tumors. Large tumors may appear as filling defects in the bladder on the cystogram phase of the urogram. Ureteral obstruction caused by a bladder tumor is usually a sign of muscle-invasive cancer. Additionally, of course, IVP can assess other upper tract abnormalities that may affect management decisions.
TreatmentTreatment for bladder cancer depends on the stage of the disease, the type of cancer, and the patient's age and overall health. Options include surgery, chemotherapy, radiation, and immunotherapy. In some cases, treatments are combined (e.g., surgery or radiation and chemotherapy, preoperative radiation).